Home / Newsletters / ITN 73 / Subscribe
Health Coverage for Kidney Transplants in the U.S.
Atul Agnihotri
Indian Transplant Newsletter. 2024 Jul-Sep; 23(3):p8-9
Print ISSN 0972 - 1568
Online ISSN 3048 - 653X
PDF
Access to health coverage for end-stage renal disease (ESRD) and kidney transplants is a lifeline for thousands of patients in the United States (U.S.). Fortunately, almost all patients in the U.S. have access to payment structures for dialysis, transplantation, and immunosuppressants utilizing a combination of private and government-funded mechanisms. Nonetheless, while the healthcare system provides substantial support, especially through federally provided Medicare, financial barriers still limit access to kidney transplantation. These barriers particularly affect living donors, whose contributions to saving lives remain underappreciated and under protected by the current US-based healthcare payment structures. This article delves into the current landscape of ESRD treatment financing in the U.S., the challenges living donors face, and the legislative efforts aimed at improving support for donors.
The Current State of Health Coverage for Kidney Transplants in the U.S.
With approximately 786,000 patients currently undergoing dialysis and around 90,000 awaiting a kidney transplant, ESRD poses a significant public health challenge in the U.S.(1) Kidney transplants account for 86% of all organ transplants in the country, with the average cost of about $150,000 per procedure and annual post-operative care amounting to over $30,000.(2) Dialysis itself costs approximately $100,000 per patient annually for the patients on Medicare, while commercial insurance pays $20,000-30,000 per month for dialysis and associated ESRD-related co-morbidity costs, making ESRD one of the most expensive chronic conditions to treat. Medicare alone spends more than $35 billion annually, 7% of total Medicare spending, on the management of ESRD patients, even though these patients comprise only 1% of all Medicare patients.(3)
In terms of coverage, U.S. patients typically rely on either public insurance programs such as Medicare, Medicaid, TRICARE, and the Veteran's Administration, or private insurance through employers or the Affordable Care Act. Medicare provides coverage for individuals over 65 and those with disabilities, ALS, or ESRD, making it a critical safety net for kidney transplant patients. The Medicare End Stage Renal Disease Program, signed into law by Richard Nixon in 1972, is one of the few disease-specific entitlement programs of the US government. For individuals with ESRD under 65, Medicare covers costs only after 33 months, during which private insurance serves as the primary payer. During this time, Medicare covers 80% of what private insurance does not pay, and the remaining 20% is borne by the patient. Once Medicare assumes primary responsibility, the roles switch with Medicare paying the first 80% of the cost and private insurance covering the remaining costs, while the patient continues to pay out of pocket costs (also called a “co-pay”). These out-of-pocket costs are capped annually so that the patient is not burdened extraordinarily, after which all the costs are borne by private insurance and/or Medicare.
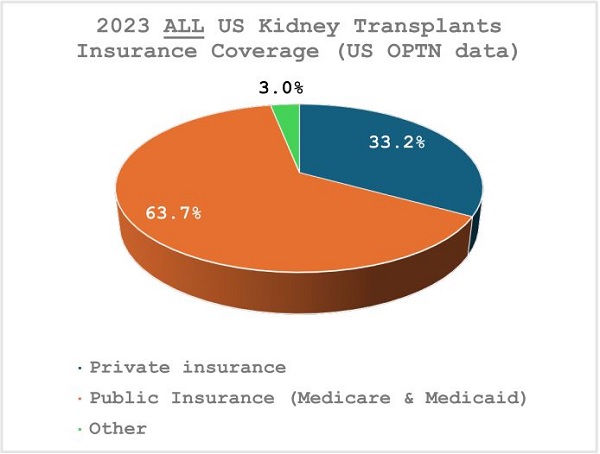
Approximately 97% of both living and deceased donor kidney transplants in the U.S. are covered by a combination of Medicare (57%), Medicaid (8%), and commercial insurance (33%).
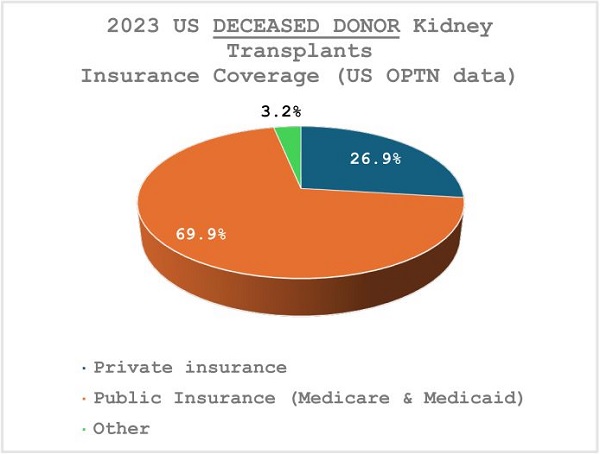
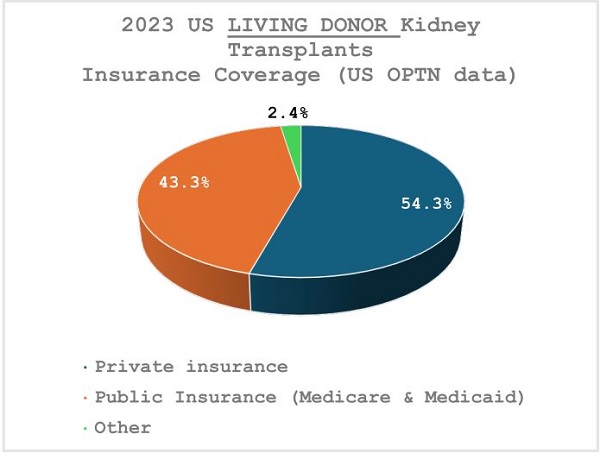
The long wait times for deceased donor transplants, typically - 5 years, mean that the majority - around 70% - of these transplants are covered by Medicare or Medicaid. In contrast, recipients of living donor kidney transplants experience significantly shorter wait times, so most of these transplants (55%) are covered by commercial insurance, though Medicare and Medicaid still account for 43% of coverage in these cases.
In January 2023, Medicare extended lifetime coverage of immunosuppressive drugs for kidney transplant recipients, whose transplants were covered by Medicare but could not secure alternate insurance support, removing the previous 36-month limit.
Challenges for Living Donors
Living donors are essential to the success of kidney transplants, providing better outcomes than deceased donor transplants and offering recipients the chance to avoid long waiting times. However, living donors often face financial burdens that are not fully covered by insurance. While recipient insurance typically covers the donor's surgery and immediate medical expenses, complications that arise more than 90 days after donation are covered by Medicare but may not be covered by private insurance. Transplant centers often negotiate with insurers or absorb these costs to protect donors from financial hardship.
Beyond the medical costs of the evaluation, surgery, hospitalization, and follow-up for living kidney donation covered by recipient's healthcare payer, donors face additional financial challenges that have been estimated to exceed $4,000 per donation.(4,5) Unfortunately, living donors must still take time off of work and often incur lost wages, travel expenses, and child/elder care costs. Despite the altruism inherent in donation, these financial barriers can deter potential donors, exacerbating the ongoing organ shortage.
The Living Donor Protection Act and Donor Protection Programs
The proposed Living Donor Protection Act represents a crucial step toward addressing the financial and insurance challenges faced by living donors. Programs like the National Living Donor Assistance Center (NLDAC) provide financial support for donors with recipients below the poverty line, and organizations like the Alliance for Paired Kidney Donation (APKD) and the National Kidney Registry (NKR) offer assistance for out-of-pocket costs to donors involved in paired exchanges.
Conclusion
While payment structures provide coverage for almost all US citizens with ESRD, challenges remain to overcome financial barriers that prevent some living kidney donations.
References:
1. 2023 United States Renal Data System (USRDS) Annual Data Report
2. Held PJ, McCormick F, Ojo A, and Roberts JP. A Cost-Benefit Analysis of
Government Compensation of Kidney Donors. American Journal of
Transplantation 16(3): 877- 885, 2016.
3. 2023 United States Renal Data System (USRDS) Annual Data Report
4. Przech S, Amit X Garg AX, Jennifer B Arnold JB, et al. Donor Nephrectomy
Outcomes Research (DONOR) Network. Financial Costs Incurred by Living
Kidney Donors: A Prospective Cohort Study. J Am Soc Nephrol. 2018
Dec;29(12):2847-2857.
5. Rodrigue JR, Schold JD, Morrissey P, Whiting J, Vella J, Kayler LK, et al.. Direct
and indirect costs following living kidney donation: findings from the KDOC
study. Am J Transplant. (2016) 16:869–76.
Available at:
https://www.itnnews.co.in/indian-transplant-newsletter/issue73/Health-Coverage-for-Kidney-Transplants-in-the-US-1342.htm
- Copyright © 2025. Published by MOHAN Foundation
