Home / Newsletters / ITN 66 / Subscribe
Heart and Lung Transplantation in India - Current Status
K R Balakrishnan
Indian Transplant Newsletter. 2022 Jul - Oct; 21(Cumulative issue 66):p6-7
Print ISSN 0972 - 1568
Online ISSN 3048 - 653X
PDF
Heart transplantation in India was first performed by P. K. Sen and colleagues way back in 1968 just a year after Christian Bernard performed the world first.(1) This was backed by prior solid experimental work on about hundred canine heart transplant experiments. This is in deed a feat which is not only remarkable but unimaginable today.(2) The patient survived only a few hours.
And after this, the wait for the first successful heart transplant was 25 years until Dr. Venugopal performed it at All India Institute of Medical sciences in August 1994.(3) The progress for the next 15 years was slow and until the year 2012 only a total of about 30 transplants had been performed in the country.
The birth of the modern heart transplant program in India happened in Chennai. The state of Tamil Nadu was the first to streamline the process of organ donation and distribution in an organized manner.(4) The previous experience of non-governmental organizations like MOHAN Foundation and NNOS to propel the government helped the state government to take the onus of the deceased donation program.(5)
This led to a steady increase in the number of donors and hearts transplanted in the state. Over the next few years, with increasing awareness, organ donation activities spread across the country. Annually close to 750 organ donations happen in India, with over 200 heart transplants. Lung transplant started in 2012 in Chennai and is now done in 3 centres in this country in significant numbers.
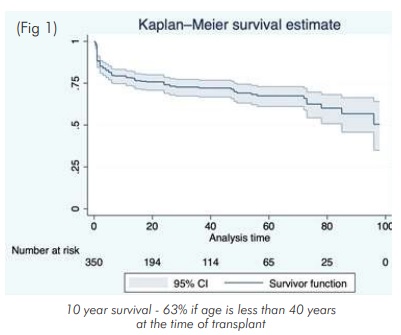
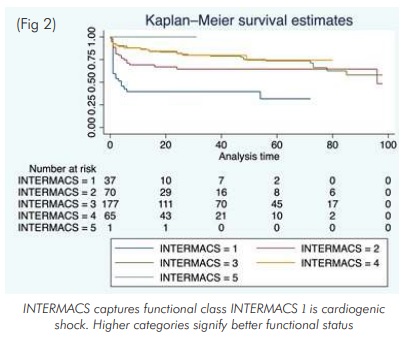
Despite the challenges of diversity and inequity in a large country, the program has matured and is growing steadily. And despite the logistic difficulties of followup including immunological monitoring, the outcomes have been comparable to programs from developed countries.(6) Our own centre results of over 500 heart transplants compare favourably with internationally published results with over 50% alive at 10 years (Fig 1). The survival is significantly better for younger recipients and patients in better functional class at the time of surgery (Fig 2).
Challenges:
1. Logistics of organ transport:
The heart as an organ is very sensitive to ischemic injury and needs to be re-perfused in the recipient within 4 to 5 hours after harvesting from the donor. This is very different from the kidney and liver where longer ischemic times are possible. Hence the logistics of transporting organs across long distances becomes a challenge in a vast country like India especially as there is no support from the insurance or the government in terms of funding for this. Very often commercial airlines are used for organ transport at exorbitant costs.(7) Several state governments cover the cost of transplants to varying extends.(8)
2. Quality of life after transplantation:
No formal exercise testing with VO2 max has been done for all the survivors. The quality of life is excellent with normal exercise capacity. A few patients have competed in transplant Olympic games and have won marathons in an open field.
3. Rejection:
Rejection is an important and potentially preventable cause of mortality both early and late. Cell mediated rejection is easier to diagnose and treat than antibody mediated rejection. Donor specific antibody testing is not available easily across the country, is expensive and often the result is available only a few days later.
Immunohistochemistry of biopsy specimens need expertise and is not always found. Our protocol of limiting endomyocardial biopsies is based on our infrastructural realities and is not a virtue in the absence of blood based immune monitoring strategies like donor derived cell free DNA estimations and Immune Cell
Function Assay (Cylex, Inc., Columbia, MD, USA) developed to measure the activity of CD4+ T cells as a marker of global immune-competence and allogene map testing. None of these tests are currently commercially widely available in India. The results presented here may be encouraging but clearly there is a great scope for improvement.
Hurdles to Overcome
1. Organ utilisation
Despite these encouraging results, the utilisation of organs, especially heart remains suboptimal and a significant number of healthy hearts and lungs remain unused.(9) Logistics of organ transport, cost, lack of trained manpower and absence of adequate infrastructure in public hospitals may be the contributing factors.
2. Late referrals
Many patients are referred after multiple admissions and procedures and after exhausting financial resources. Mechanical circulatory support, even though a well-established therapeutic modality in India, is very expensive and not covered by insurance.
3. Pediatric organ donations:
They are very few and no donation is currently happening in public children's hospitals and often hearts from older donors are used in children. Older donor age is associated with poorer long-term survival, a highly unsatisfactory situation.(10)
4. Lack of heart failure clinics
Heart failure cardiology as a subspecialty needs to be promoted to compete with more lucrative interventional cardiology streams.(11) More awareness needs to be created for increasing organ donation rates and for earlier referrals for optimal outcomes. The involvement of cardiologists in this program is still suboptimal and a large number of patients who might have benefitted from the available organs are denied this life saving therapy.
Conclusion:
Heart and lung transplantations are now well established procedures with long term results comparable to published international results. The learnings from India will help many countries to fast forward their program in the region. Despite the multiple challenges India's thoracic organs transplant program has over the years matured and is an example for other developing countries to follow.
References:
1. David S Jones, Kavita Sivaramakrishnan, Transplant Buccaneers: P.K. Sen and India's First Heart Transplant, February 1968, Journal of the History of Medicine and Allied Sciences, Volume 73, Issue 3, July 2018, Pages 303–332.
2. Sen PK, Parulkar GB, Panday SR, Kinare SG. Homologous canine heart transplantation: a preliminary report of 100 experiments. Indian J Med Res. 1965 Jul;53(7):674-84.
3. Venugopal P. The first successful heart transplant in India. Natl Med J India. 1994 Sep-Oct;7(5):213-5.
4. Annadurai K, Mani G, Danasekaran R. Road map to organ donation in Tamil Nadu: An excellent model for India. Int J Prev Med 2015;6:21.
5. Kanvinde, Hemal; Shroff, Sunil; Kumar, Pallavi; Jairam, Jaya. Experiences and Challenges in an NGO run Organ Donation Helpline. Transplantation: July 2018 - Volume 102 - Issue - p S197 doi: 10.1097/01.tp.0000542846.76127.c2
6. Balakrishnan KR, Sureshrao KG, Ravikumar R, Muralikrishna T, Ganapathy Subramaniam K, Mohan R, Ajay A, Ramasubramanian K, Jagdish D, Veena R. Medium term results following heart transplantation for end stage heart failure: A single center experience of 257 patients. Indian Heart J. 2020 Nov-Dec;72(6):524-534. doi: 10.1016/j.ihj.2020.09.010.
7. K. Bala Krishnan, K. Suresh Rao, M.K. Tanguturu, M. Rajam, A. Aravind, J. Dushyanthan, R. Subramanian, V. Ramanan, Commercial Airlines as a Viable, Safe and Cost Effective Way for Transporting the Donor Hearts across the Country: Single Center Experience, The Journal of Heart and Lung Transplantation, Volume 38, Issue 4, Supplement, 2019, Pages S133-S134, ISSN 1053-2498
8. https://timesofindia.indiatimes.com/city/chennai/heart-transplant-performed-for-first-time-in-coimbatore-under-chief-ministers-comprehensive-health-insurance-scheme/articleshow/67469077.cms
9. https://jeevandan.gov.in/organstatistics.htm
10. Balakrishnan KR, Rao KGS, Subramaniam GK, Tanguturu MK, Arvind A, Ramanan V, Dhushyanthan J, Ramasubramanian K, Kumaran KS, Sellamuthu G, Rajam M, Mettur S, Gnansekharan P, Ratnagiri R. Clinical profiles and risk factors for early and medium-term mortality following heart transplantation in a pediatric population: A single-center experience. Ann Pediatr Cardiol. 2021 Jan-Mar;14(1):42-52.
11. Balakrishnan K. Heart transplantation in India-are we there yet? Indian J Thorac Cardiovasc Surg. 2020 Aug;36(Suppl 2):159-165.
Available at:
https://www.itnnews.co.in/indian-transplant-newsletter/issue66/Heart-and-Lung-Transplantation-in-India-Current-Status-1186.htm
- Copyright © 2025. Published by MOHAN Foundation
