
Lung Transplant Program In India : Progress & Future
Unmil Shah, Transplant Pulmonologist, Inst. of Heart & Lung Transplant, KIMS, Secunderabad & Sir H N Reliance Hospital, Mumbai
Sandeep Attawar, Program Director & Transplant Surgeon, Inst. of Heart & Lung Transplant, KIMS, Secunderabad & Sir H N Reliance Hospital, Mumbai
Introduction:
Lung transplantation (LTx) is now a well-accepted treatment option for a variety of selected end-stage lung diseases(ESLD) which improves survival rates and quality of life. The International Society for Heart and Lung Transplantation Registry reports a 1 and 5-year survival of 85% and 59%, respectively, for adult lung transplant recipients transplanted since 2010.[1]
The current indications of LTx are, but not limited to, chronic obstructive pulmonary disease (COPD), interstitial lung diseases (ILDs), cystic fibrosis (CF), non-CF bronchiectasis, and pulmonary hypertension. LTx is not usually considered in patients with acute lung injury (ALI) due to any infectious cause. However, there has been a paradigm shift in the treatment strategy in the cohort of ALI due to COVID-19.[1]
Three methods of LTxs are possible. These are single lung transplant through posterolateral thoracotomy, double lung transplant with a clamshell incision, and combined heart and lung transplant as enbloc through median sternotomy.
Lung Transplant in India :
The first HLTx in India was performed by Dr K M Cherian and group in 1999 [7]. On July 11, 2012, Dr. Jnanesh Thacker, performed the first successful lung transplant in India. Subsequent to this, there were few reports of heart and lung or lung transplants discretely in the first ten years. [1]
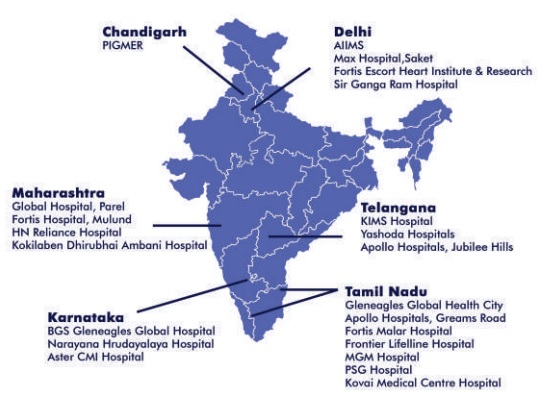
At present, there are a few lung transplant centers in India which cover a wide geographic area (Fig. 1).[1] Yet some major challenges remain, such as inappropriate timing of referrals, distance to the referring hospitals, lack of infrastructure, social taboo associated with organ donation, and lack of coordination between different centers.
Challenges in Indian settings at present :
1) At donor level : Poor organ donation rates
2) At recipient level : Delayed referrals
3) At logistics : Remote areas of retrieval, Charter flight options, etc
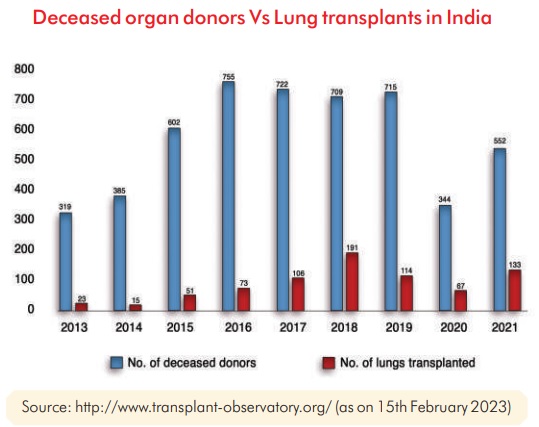
Organ Donation in India : As per GODT, there were 552 (0.4pmp) actual deceased donors in 2021 as compared to 715 in 2019 (0.52 pmp) pre-COVID pandemic. 133 lung transplants happened in 2021 as compared to 114 in 2019, pre-COVID pandemic.[2]
The rise in Lung Transplants has been partly attributed by the COVID pandemic which led to few select patients with Post-COVID ARDS, end stage lung disease requiring lung transplant and also because awareness among medical fraternity regarding availability of lung transplant services.
Future in Lung Transplant :
In view of more number of extended criteria donors, there was a need for research regarding expanding donor pool. Hence, came two game-changing concepts which when applied were able to increase donor pool, helping in turn to reduce wait-list mortality. These are (a) Ex Vivo Lung Perfusion (EVLP) and (b) Donation after Circulatory Death (DCD).
a) EVLP: This is a technique used to evaluate and screen compromised donor lungs with potential for recovery. This technique has been already used in LTx centres across the world. EVLP can restore the circulation and ventilation of the ex vivo lung. At an ambient temperature of 37°C, a membrane oxygenator is used to simulate oxygen consumption in the body via deoxygenation and maintain the physiological state of lungs with specific perfusate and ventilation. EVLP is currently used mainly to evaluate certain high-risk donor lungs. It is mainly indicated for (I) an oxygenation index <300 mmHg; (II) pulmonary oedema as indicated by the last chest X-ray; (III) collapse or poor expansion of a donor lung during harvest; (IV) blood transfusion >10 U; and (V) lungs from donors with cardiac death. EVLP is not suitable in cases of apparent pneumonia, severe mechanical lung injury (including multiple lobar injury) or significant aspiration of gastric contents. [3]
EVLP: will help optimise marginal lungs before implanting, thus improving outcomes and increasing donor pool.
b) DCD: Here, organs are removed from donors after cardiac arrest. DCD can be considered in a patient who does not fulfil brainstem death criteria, but has no hope of recovery, and it is in the best interest of the patient to withdraw life-sustaining treatment. The main difference between DCD and donation after brainstem death (DBD) organs is the warm ischemia time. Warm ischemia will be minimal in DBD donors as compared to DCD donors, where there is an interval after asystole where organs are not being perfused and have not yet been cooled, leading to relatively longer warm ischemia time. In India, the concept of DCD is evolving, with want of more legal clarity regarding withdrawal of life support. When decision to withdraw treatment support has been taken by the family and the physician, discussion regarding organ donation can be initiated.[3]
DCD : will help increase the donor pool and will lead to reducing waitlist time in future.
Other Recent Advances in Lung Transplant
c) Cell-free DNA (cfDNA) is released from cells into the surrounding tissue and bloodstream during apoptotic and necrotic cellular decay and can be detected in plasma and serum. An association exists between circulating levels of cfDNA and acute lung injury, sepsis, and malignant disease. Improved technical development has made it possible to differentiate donor-derived cfDNA (dd-cfDNA) from recipient-derived cfDNA (rd-cfDNA) in the bloodstream. Thus, quantification of each portion can be made, and the ratio of dd-cfDNA to all cfDNA, also called the donor fraction (DF), has been associated with graft injury after kidney, liver, heart and lung transplantation. [4]
%ddcfDNA significantly increased at the time of histopathological grade moderate or severe ACR (ACR grade ≥ 3) vs stable controls. A threshold dd-cfDNA level of >1% demonstrated 100% sensitivity and 73% specificity for the diagnosis of moderate or severe ACR with an area under the receiver-operating characteristic curve (AUC) of 0.9. Taking the available evidence into account, dd-cfDNA, reported as %ddcfDNA appears to demonstrate good diagnostic accuracy for the diagnosis of acute rejection in lung transplant patients. [5]
This test will in future reduce the need for frequent lung biopsies post lung transplant to monitor rejection.
d) ECP : Extra-corporeal Photopheresis : Data from these studies suggest that ECP therapy is associated with improvement or stabilization in lung function and sustainable, statistically significant decreases in the rate of lung function decline in patients with Bronchiolitis Obliterans Syndrome (BOS).
Furthermore, two studies reported that 25% to 30% of patients with BOS have an improvement in lung function after treatment with ECP. Extracorporeal photopheresis was generally safe and well tolerated. [6]
ECP : might become an important modality to treat CLAD where not much successful options are available.
Conclusion : Lung transplantation is still the only option that can be offered to the majority of selected end-stage lung disease patients with presumed modest improvements in quality-adjusted survival. India will need to have multipronged approach to improve organ donation rates, to create awareness for Early Referrals for optimisation, to incorporate services like EVLP, ECP, ddcfDNA, etc which are going to be game changers in the field of lung transplantation.
References :
1. Attawar S, Manoly I, Shah U. Lung Transplantation in India: a Brief Review, Landmarks, Indian Scenario, and our Experience. Indian J Surg. 2023 Jan 16:1-12. doi: 10.1007/s12262- 023-03663-w. Epub ahead of print. PMID: 36686557; PMCID: PMC9841148.
2. https://www.transplant-observatory.org/summary/
3. Shah UB, Kumar P, Rahulan V, Dutta P, Attawar S. Challenges of lung transplantation in India. Indian J Thorac Cardiovasc Surg. 2022 Jul;38(Suppl 2):229-236. doi: 10.1007/s12055-021- 01170-9. Epub 2021 Apr 24. PMID: 33935383; PMCID: PMC8064884.
4. Magnusson JM, Ricksten A, Dellgren G, Wasslavik C, Nordén R, Westin J, Boehmer J. Cell-free DNA as a biomarker after lung transplantation: A proof-of-concept study. Immun Inflamm Dis. 2022 May;10(5):e620. doi: 10.1002/iid3.620. PMID: 35478446; PMCID: PMC9017613.
5. Keller M, Agbor-Enoh S. Donor-Derived Cell-Free DNA for Acute Rejection Monitoring in Heart and Lung Transplantation. Curr Transplant Rep. 2021;8(4):351-358. doi: 10.1007/s40472-021-00349-8. Epub 2021 Nov 5. PMID: 34754720; PMCID: PMC8570240.
6. Hachem R, Corris P. Extracorporeal Photopheresis for Bronchiolitis Obliterans Syndrome After Lung Transplantation. Transplantation. 2018 Jul;102(7):1059-1065. doi: 10.1097/TP.0000000000002168. PMID: 29557913; PMCID: PMC7228625.
7. Madhu Sankar N, Kurian VM, Rajan S, Ninan B, Ajit M, Cherian KM (2003) Heart-lung transplantation in India: initial experience. Indian Heart J 55(2):185–187
- Shah U, Attawar S., . Lung Transplant Program In India : Progress & Future. Indian Transplant Newsletter. Vol.22 Issue 67, November 2022 - February 2023
- Shah U, Attawar S., . Lung Transplant Program In India : Progress & Future. Indian Transplant Newsletter. Vol.22 Issue 67, November 2022 - February 2023. Available at:
https://www.itnnews.co.in/indian-transplant-newsletter/issue67/Lung-Transplant-Program-In-India-Progress-Future-1208.htm
